Gluten Intolerance vs. Celiac Disease: A Comprehensive Guide
Gluten Intolerance vs. Celiac Disease
In the world of gluten sensitivity disorders, two conditions often get intertwined – gluten intolerance and celiac disease. While both conditions may share common symptoms, they have distinct causes that are essential to understand for accurate diagnosis and proper treatment. This comprehensive guide will help clarify the differences, key celiac symptoms, and how to manage them effectively.
Celiac Disease: An Autoimmune Disorder
Celiac disease, also known as coeliac disease or gluten-sensitive enteropathy, is a serious autoimmune disorder that impacts the digestive system. An autoimmune disease means that the body’s immune system mistakenly attacks its own healthy tissues. In the case of celiac disease, the immune system reacts to gluten, a protein found in wheat, barley, and rye, and launches an attack on the lining of the small intestine. When individuals with celiac disease consume gluten, their immune system attacks the small intestine, leading to villous atrophy. This damages the villi, impairing nutrient absorption and causing a variety of symptoms.
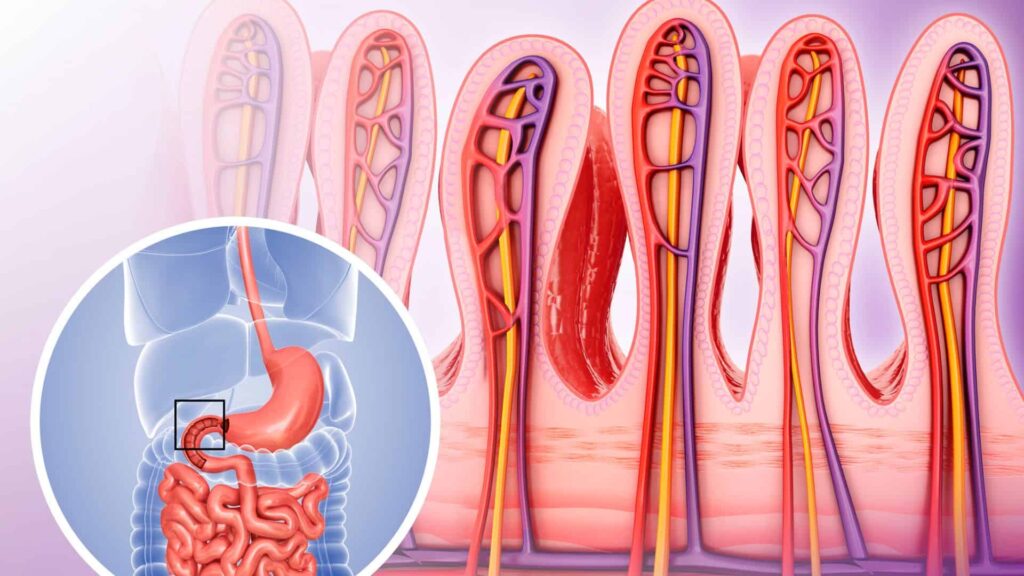
To diagnose celiac disease, a combination of blood tests, a physical exam, and an evaluation of digestive symptoms and family history are typically performed. Blood tests can detect specific antibodies produced by the immune system in response to gluten consumption. If the blood test results indicate a positive reaction, further testing, such as an endoscopy with a biopsy of the small intestine, may be recommended to confirm the diagnosis and check for damage or villous atrophy.
It’s important to note that celiac disease is not a food allergy, which typically triggers an immediate and severe allergic reaction like difficulty breathing or a life-threatening anaphylactic response. Instead, celiac disease is an autoimmune condition that can cause various digestive symptoms, nutritional deficiencies, and common symptoms like fatigue, joint pain, and skin rashes when consuming even small amounts of gluten.

While the exact cause of celiac disease is not fully understood, it is believed to be influenced by both genetic predisposition and environmental factors. Individuals with a family history of celiac disease or other autoimmune conditions among first-degree relatives may have a higher risk of developing the condition.
In the United States, celiac disease affects approximately 1% of the population, although many cases may go undiagnosed due to the wide range of potential symptoms and the similarity to other digestive conditions. Adhering to a strict gluten-free diet, which involves avoiding all gluten-containing foods, is the only treatment for managing celiac disease and preventing severe symptoms or complications.
Read more about your child’s diagnosis.
Gluten Intolerance vs. Celiac Disease – Symptoms
While both conditions result in gluten intolerance symptoms like stomach pain, bloating, and fatigue, celiac disease often causes more severe symptoms, including swollen gums and muscle spasms due to nutrient deficiencies. In contrast, non-celiac gluten sensitivity (NCGS) presents similar gluten intolerance signs but without the immune response seen in celiac disease.
- Celiac Disease Symptoms:
- Chronic diarrhea
- Nutrient deficiencies such as anemia and osteoporosis
- Abdominal pain
- Fatigue and joint pain
- Gluten Intolerance Symptoms:
- Abdominal pain
- Headaches
- Fatigue
- Swollen hands
- Skin rashes
The Diagnosis Process Gluten Intolerance vs. Celiac Disease
To confirm a celiac disease diagnosis, healthcare providers use blood tests, an endoscopy, and sometimes genetic testing to look for specific genes associated with coeliac disease. For NCGS, an elimination diet is typically used to assess gluten sensitivity and whether gluten is causing allergy symptoms. This diagnosis process is key to avoiding further intestinal damage in celiac patients.

It’s important to note that self-diagnosis and self-treatment can be risky, as these conditions may have similar symptoms to other medical issues. Working with a healthcare provider is essential for an accurate diagnosis and appropriate treatment plan.
Managing Gluten Intolerance and Celiac Disease
While the underlying causes of celiac disease and non-celiac gluten sensitivity differ, the primary treatment for both conditions is a strict gluten-free diet. This means avoiding all gluten-containing grains, such as wheat, barley, and rye, and carefully reading food labels to identify hidden sources of gluten.
For individuals with celiac disease, adhering to a gluten-free diet is crucial to prevent further intestinal damage and nutrient deficiencies. Untreated celiac disease can lead to serious complications, including osteoporosis, infertility, and an increased risk of certain cancers.
In the case of NCGS, following a gluten-free diet can alleviate symptoms and improve overall well-being. However, it’s important to note that some individuals may also need to avoid other foods or substances that can cause reactions, such as dairy, soy, or certain additives.
Read more about guidance for a gluten-free diet.
Support and Resources
Living with gluten-related disorders doesn’t have to be challenging. Access to reliable gluten-free info, grocery lists, and a meal planner can make managing a gluten-free lifestyle much easier. Additionally, joining support groups or working with a registered dietitian can help individuals navigate gluten-free recipes, safe foods, and gluten allergy concerns. Understanding what gluten is and reading food labels carefully is key to living a healthy, gluten-free life.
Gluten Intolerance vs. Celiac Disease – Conclusion
While gluten intolerance and celiac disease share some similarities in their symptoms, they are distinct conditions with different underlying causes and implications for overall health. Understanding the differences between these two conditions is crucial for receiving an accurate diagnosis, following the appropriate treatment plan, and managing symptoms effectively. By working closely with healthcare providers, seeking support, and adhering to a strict gluten-free celiac diet (when necessary), individuals with gluten-related disorders can improve their quality of life and minimize the risk of potential complications.